Click HERE for patient information leaflet
What is a retinal detachment?
A retinal detachment happens when the retina comes away from the wall of the eye.The retina is the light sensitive 'film' in the camera that is the eye. It can come off for several reasons most commonly because the Jelly pulls a small tear in the retina but it can also be pulled off as in patients with diabetes and sometimes fluid under the retina pushes it off. The jelly pulling is by far the most common. As the retina detaches the vision becomes grey. If the retina detaches at the centre of the retina (the Macula) then vision becomes very poor, if all the retina detaches all sight is lost.
Why has this happened?
The Jelly of the eye is really useful when you were in your mothers tummy (ok uterus!!). After birth I am afraid it just degenerates, fluid pockets appear, clumps of gel form and these are what we call 'Floaters'. With time the fluid increases, the constant moving of the eye swishes this about and slowly the contact between the retina and the jelly weakens until eventually it separates (Posterior Vitreous Detachment or PVD). In short sighted people this happens a lot earlier and they are more at risk of a failure of the jelly to separate from the retina resulting in a flap of retina lifting away causing a tear (Imagine grabbing some wall paper and pulling, you will get a small tear). As jelly pulls on the retina the retina Flashes. As the retina tears it may bleed or pigment is released from under the retina and these bits suddenly float around, Floaters. If you get to us at this point we can usually sit you down in clinic and laser the tear around sticking the retina down and preventing the next stage. With a tear, the seal on the vacuum packed retina is broken and fluid starts to get underneath and this progresses the retina stops working and you get Fading vision.
What can be done?
It is likely you are reading this after the event because we generally like to get on with fixing retinal detachments as soon as we can. Ideally we want to repair the retina before the macula comes off, once the macula is off we want to fix it within 7 days but generally aim to get it done as soon as we can. If the retina has been off months we will repair it on the next available slot on our elective lists.
It is helpful to think of wallpaper and walls when it comes to fixing a retinal detachment. The wall is the wall of the eye and the wallpaper is the retina. The aim is to find the holes or tears in the wallpaper, seal them with laser or freezing and then get the wallpaper and the wall back in contact. We can do this by pushing the wall in towards the wall paper by using a silicone buckle sutured onto the outside of the eye (a buckle), or we can take the Jelly out of the eye and push the wall paper against the wall from the inside (a vitrectomy). Once the two are in contact we apply a 'glue' (laser or freezing therapy)which work by causing scar tissue which knits the two layers together. In general if you are young and the jelly has not separated from the retina I tend to use a buckle otherwise I do vitrectomy.
In vitrectomy, the jelly is removed by a tiny guillotine which cuts the jelly into tiny pieces 5000 times a minute and then sucks it away. A salt water drip keeps the eye inflated during this removal. At the end of vitrectomy the sealed retina needs to be kept dry and so I put in a tamponade which is usually a gas that will last between 2 weeks and 2 months. Sometimes oil is used if the detachment is complex. You cannot see through gas and you cannot fly with gas in the eye. You can see vague shapes through oil but you can fly with oil. As the gas leaves the eye the shadow gets smaller, rounder and lower until it suddenly disappears, oil requires a second operation to remove it.
A buckle is put on the outside of the eye and the Jelly is left well alone. The success rates quoted have hidden problems in terms of case selection and definition of success but seem to sit around 80%-85%. Around 6-8% of people get an exaggerated scarring response we call PVR (Proliferative vitreoretinopathy) and this pulls the retina off and sometimes requires several operations to overcome and it the main cause of failure. We cannot predict who will get PVR but if you do nothing it is very likely to develop.
Both operations are carried out under a local anaesthetic with the eye numb and unable to move. It should be comfortable throughout and if you need a little 'chemical courage' we can give sedation. The operation takes around 45 minutes to complete but can be longer or shorter depending on complexity.
Should I have it done?
Nobody jumps out of a second floor window, If a Lion walked into the room most would jump! This is the largest lion you have ever seen. Your back is against the wall, if you choose to do nothing then you will lose all sight in the eye and the eye might become painful and shrunken so jump please.
Proliferative Vitreo-Retinopathy (PVR)
What is PVR?
About 6-8% of patients with retinal detachment go on to develop PVR. We do not know why, we do not know how to prevent it. If you imagine a fresh retinal detachment is like thin wall paper coming off the wall of the eye and our job is to push it back on and it goes back smoothly. Take a piece of paper and lift the corner and then let go, the paper falls onto the surface perfectly. In PVR the retina becomes scarred. This can be on the surface, underneath or even within the retina itself. It becomes like cardboard and will not go back against the wall of the eye. Take your piece of paper and scrunch a corner and now let it go. It does not fall back smoothly, there are lumps and bumps and gaps, this is PVR.
How do we treat it?
Surgery for this is demonstrated to the left. The retina is scrunched up with multiple folds and ridges. Our first job is to try to peel any surface scar tissue and in this case there was surface membrane to peel. We stain it with blue and then pick and peel it off. The retina becomes more mobile as the scar tissue is released. Next some heavy liquid is placed into the eye to start to roll the retina flat and it acts as a second hand to help further peeling of scar tissue. There comes a point when the retina is too tight to put back and this is cut away. At one stage the fellow pushes on the eye whilst I was operating (He was meant to, it is called indented vitrectomy!!) and caused a bleed but this was dealt with quickly and all was well! The new edge is lasered in place and then oil is placed into the eye and left for two months. In this case the retina remained attached and with a scleral haptic fixated lens this man got back the top three lines of the test chart, so very blurred but very useful. Surgery is under a local anaesthetic and took around an hour and a half to complete. If you get PVR then be prepared for a series of operations and potentially a poor outcome but remember if you do nothing PVR is likely to develop anyway and the eye can become soft, shrunken painful and blind so surgery is certainly the way forward.

|
Sub retinal surgery Ab Externo From outside!.mp4 Size : 23966.669 Kb Type : mp4 |
Failed Buckle surgery with Sub retinal Surgery to remove subretinal bands
Thanks to ST for allowing me to publish her surgery. She presented with a chronic retinal detachment from trauma. Central vision had been lost and it had been there for so long that scarring was occurring under the retina. I proceeded to a buckle to avoid Vitrectomy and the issues with cataract and further scarring. Although the buckle was well placed the retina was held up by the subretinal bands. Think of a sheet over a washing line being draped over andheld up. I would usually resort to Vitrectomy, make a hole in the retina over the bands, pull them out, heavy liquid to flatten retina, Laser and then oil. The oil would need to be removed with a second operation. I decided to try a subretinal approach from the outside, a technique developed by my good friend Bernard Wolff in South Africa (Thanks Bernard!) In this technique the vitrectomy port is place way back so that it enters the eye under the retina (We usually avoid this!). By going a long way back the port enters under the retina where it is detached so no harm done to the retina. Once in this space the bands can be removed and the fluid drained and the retina re attached. Then laser is applied to keep it in place. The procedure took half an hour rather than an hour plus. There is very little risk of cataract as the gel has been left in place. The procedure was under a local anaesthetic with some sedation.
Update: 22/3/17. Retina attached and vision now 0.52 which is very good considering the chronic nature of the detachment which was macular off. I am sure this will improve over the next year.
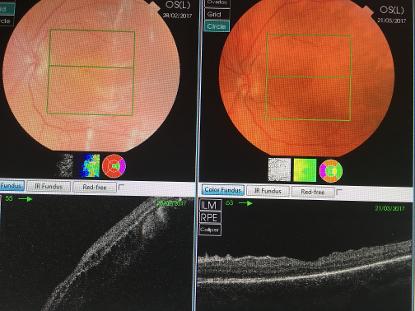
The picture on the left shows the OCT scans before (left) and after (right) surgery. The left side (before surgery) clearly shows the white bands running from top to bottom. These are the sub retinal bands that were holding the retina off the wall of the eye in spite of a well positioned buckle (See video). On the right, the retina is attached and the bands have gone.
These lower images are cross sections through the retina at the level of the green line above. On the left the retina is 'up in the air' and well detached. On the right you can see the retina has landed back onto the thick white line (the RPE), the retina is attached.

|
Scleral Buckle.mp4 Size : 19377.884 Kb Type : mp4 |
Scleral Buckle for retinal detachment
Ok I admit it. I usually argue that eye suregy is beautiful and suitable for all the family to watch (!!?)but a buckle is not for the faint hearted. It involves some blood and muscles exposed and is just not pretty. However it was how most detachments were treated in the past (After sticking a blade into the eye and then using a hot stick!) To fix a retinal detachment we need to close the break and relieve traction. Vitrectomy pushes the wall paper against the wall, a buckle pushes the wall against the wall paper. Surgery is carried out under local anaesthetic with some sedation and takes around 1 hour to complete. It is a dying art with less and less buckles perfomed. Sucess rates are similar to Vitrectomy in the published literature but one advantage is we stay outside the eye reducing some of the risks of vitrectomy. However there are risks of double vision and change in spectacle prescription. I use in young people with limited detachments.
Thanks to T for allowing me to share his surgery. He came in with loss of vision in one eye. He has Sticklers and very high myopia (18 D plus). He was due to start GCSEs later that week (as was my son) so I got the stress in his situation! He had a total retinal detachment with early scarring as it had been present for some time but given his poor sight he had not noticed. An alternative treatment would have been an encircling band but given his age, his early scarring and his high myopia I elected to do vitrectomy. Surgery was slow but went well and I was able to peel the surface membranes and the retina re attached under air. I used oil given the complex nature of the detachment to keep my options open should it fail. Oil came out after 6 weeks and the retina has remained attached. I saw him last week with his second eye detached and so we will get him through this and then remove the cataract in his first eye. I am hoping to free him of very thick spectacles.